Open Enrollment is Oct 1-31. To choose Empower, call 1-833-402-0672
Frequently Asked Questions
54 results
-
Members
What is a care coordinator?
A care coordinator will connect you and your family with community supports, doctors, or coordinate the services you are already receiving, or any additional support needed. They will write a Person Centered Service Plan (PCSP) to help you achieve your goals and link your medical health, developmental disability, and specialty health services.
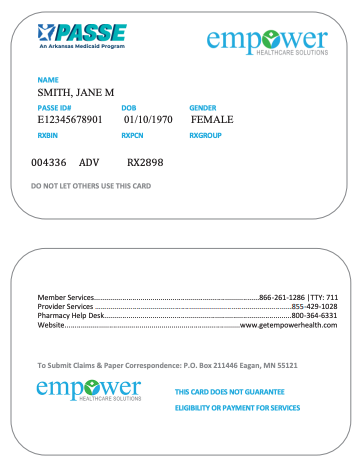
What if i have not received my Empower ID Card? How do i get my Empower ID?
You can call Empower Member Services Toll Free 24/7 at 866-261-1286 to get your member ID number and request a replacement card. You can also print your Empower ID card from the Manage My Account Portal.
How do I find an Empower pharmacy?
Click on “Find a Pharmacy” under the For Members tab. All CVS/Caremark pharmacies are in-network with Empower. Prescription information is on your Empower Member ID card.
What if my provider tells me they are not in network with Empower?
Providers may choose not to participate in the PASSE. If this happens, contact your care coordinator so they can help you find another Provider. Out of Network providers can choose to see Empower Members and bill Empower for that service.
What is this new PASSE program?
Empower is a PASSE (Provider-Led Arkansas Shared Savings Entity). The PASSE is a new Medicaid program to address the needs of people who have behavioral health, intellectual disability, or developmental disability service needs.
How can I contact Empower?
You can call Empower Member Services Toll Free 24/7 at 866-261-1286 I TTY: 711 or by emailing empower@empowerarkansas.com. You can also contact your Care Coordinator directly or by emailing CareCoordination@empowerarkansas.com.
I would like to share my opinion about care, how can I do that?
Empower cares about the services we provide. If you are not happy with any part of your care, please call us at 866-261-1286 I TTY: 711 or email complaintsandgrievance@empowerarkansas.com. If the issue or complaint cannot be resolved to your satisfaction, please contact the DHS PASSE Office of the Ombudsman at 844-843-7351, individuals who have a hearing or speech impairment can contact 888-987-1200, option 2 or PASSEOmbudsmanOffice@dhs.arkansas.gov.
We developed a Consumer Advisory Council (CAC) to ensure people have the opportunity to provide meaningful feedback and important program information across the state. The CAC also helps guide our mission to empower individuals to lead fuller, healthier lives at home and in their communities.
Empower invites our members to meet with us in person to share their opinions. During this meeting, members tell us what they think about our program. Empower uses this information to make program changes based on members’ needs. If you have feedback please contact our Consumer Advisory Council by email at Consumer.Advisory@empowerarkansas.com.
What does being a member of Empower mean for me?
Empower will be managing your Medicaid benefits. You will be assigned a Care Coordinator who will contact you within 15 business days.
How did you get my information? Who referred me to this program?
If you or your family member receives Medicaid and need a high level of behavioral health services, receive developmental disability services through the waiver, or you are on the waiver wait list you should have been contacted for an Arkansas Independent Assessment (ARIA). The Department of Human Services (DHS) enrolled you as a member of Empower based on responses on the ARIA. These answers helped DHS assign you to a level – or tier – of service to meet your needs. If you were assigned a Tier 2 or 3, you were assigned to a PASSE.
Will I lose my benefits if I do not participate in a PASSE?
You are assigned to a PASSE to manage your Medicaid benefits and organize your care if you are a Tier 2 or Tier 3.
How do I know what Tier level I was assessed as by the Independent Assessment?
Members should have received a packet from Optum with their Tier results and a report of needs. If you did not receive this information, contact Optum at 844809-9538.
What if I do not agree with my Tier?
If you do not agree with your tier determination, you have the right to request a hearing. A request must be received at the DHS Office of Appeals and Hearings’ address below no later than 35 days from the mailing date. Please put your request for a hearing and for any services in writing. With your request, please include a copy of your assessment results from Optum and mail it to:
Arkansas Department of Human Services
Office of Appeals & HearingsP.O. Box 1437, Slot N401
Little Rock, AR 72203
Division of Medical ServicesIs the Empower ID card going to take the place of my Medicaid card?
You need to take your Empower ID card to any provider you use for medical, pharmacy, behavioral health or developmental disability services beginning March 1, 2019.
Will there be a copay?
No, providers are not allowed to bill members for any covered services provided. See your member handbook for a list of covered services.
What if my provider is not a provider in the Empower network?
All providers are encouraged to join every PASSE so they can see members from every PASSE. If your provider is not in Empower’s Network and you would like them to be, please let your Care Coordinator know, or email our Provider Relations team at EmpowerPR@empowerarkansas.com.
How can I talk with my Care Coordinator if I need an interpreter or special services?
Contact Empower at 866-261-1286 or let your Care Coordinator know if you need an interpreter or other services to help with communication. This includes sign language interpreters, translation services including interpreters, and written information in other languages or formats such as large print, audio, and other electronic formats.
What services will be covered for Empower Members?
You will have access to the same services covered by Medicaid today. They will be covered as long as those services are medically necessary. Dental services are currently excluded from the PASSE and you will continue to use your Medicaid dental ID card to receive any covered dental services.
What services will not be covered for Empower Members?
Below is a list of services that Empower does not cover.
- Services that are experimental or investigational in nature
- Services that are provided by a provider that is not in the Empower network, unless Empower has given prior authorization
- Services that are provided without a required prior authorization
- Elective cosmetic surgery
- Infertility care
- Any service that is not medically necessary
- Services provided through local education agencies
- Extended stays in special needs facilities or nursing homes
- Other services excluded from the PASSE:
- Nonemergency transportation (NET)
- Dental benefits in a capitated program
- School-based services provided by school employees
- Skilled nursing facility services unless it is rehabilitative in nature
- Assisted living facility services
- Human Development Centers (HDCs)
- Waiver services provided to the elderly and adults with physical disabilities through the ARChoices in Homecare program or the Arkansas Independent Choices program
- If you are unsure if a service is covered, call Member Services at 866-2611286 I TTY: 711.
How do I get a Primary Care Physician (PCP)?
Members select their PCP when they sign up for Medicaid. Members who are also eligible for Medicare are able to keep their Medicare PCP. For any members who do not select a PCP, Empower will automatically assign a PCP based on:
- the member’s claims history (who they have seen in the past);
- a member’s geographical location;
- appropriate distribution by provider (so that members are not overly concentrated with the same PCP).
Members ages 18 and older will be assigned to a general or family practitioner, internal medicine, or other specialty provider approved by the state. Members under 18 years old will be assigned to a pediatrician or family practitioner. At any time, a member can call Empower Member Services and request that their PCP be changed, and Empower will honor that request if they are an In-Network provider.
How do I know if I am a member of Empower?
Empower members will receive a welcome packet that contains:
- member welcome letter
- a member identification (ID) card
- how to locate the member handbook on our website
- how to find the provider directory on our website
You can also call our Customer Service line at any time to verify your eligibility at 866-261-1286 I TTY: 711.
Can you help us pay our bills? (light bill, gas bill)
Your Care Coordinator can connect you to resources in your community that help with these needs.
Are you taking the place of our DCFS caseworker?
No, we are not replacing your DCFS caseworker or any provider you have. You will have a care coordinator to ensure all services are coordinated and organized.
Do you have to come to our home every month?
Empower Care Coordinators are working with you and your family to obtain the best possible outcomes. Meeting face to face can enhance communication and help our Care Coordinators coordinate between you and your service providers. Some of your meetings will be face to face while other visits will be on the phone. Your care coordinator will work with each individual member to schedule visits at the time and place that is easiest for you.
What services do you offer?
See your member handbook for covered services. The member handbook is available to all members or can be found on the Empower website at www.getempowerhealth.com/for-members/member-materials/member-handbook/.
Do you have to call every month? Why?
Yes, we want to ensure all services are coordinated. Your care coordinator will also assist with any care related issues. If you would like to talk about the way that your care coordination contacts you, speak with them directly.
Do you go to the school to speak to teachers?
Care Coordinators will only speak with individuals at a member’s school when members/guardians have agreed to it. It may be helpful to have your Care Coordinator attend your child’s Individual Education Plan (IEP) meetings.
Do you call the doctor’s office?
Empower can assist you with calling your doctor’s office, if needed. Care Coordinators will only speak with individuals at a member’s doctor’s office when members/guardians have agreed to it.
What is the Person Centered Service Plan (PCSP)?
Empower members have a Person Centered Service Plan (PCSP). The Care Coordinator gets copies of all treatment and service plans for members from providers. The goal is to prevent duplication of services, ensure timely access to all needed services, and identify any service gaps, as well as provide any health education or health coaching identified. The PCSP is made when you, your family, and your providers work together to meet your needs. It is to make sure you have supports that know your background and the services you receive and may need.
How do I get my pharmacy information?
Your Empower ID card will include the necessary information for your pharmacy to fill a prescription under your benefit plan. Show your new ID card to the pharmacy before filling your first prescription in order to avoid any prescription delays.
Will my prescription costs change?
There will be no cost to you for prescriptions with Empower.
What if I take a medicine that requires Prior Authorization?
For those medicines listed on the formulary as Prior Authorization required, a request from your provider prescribing the medication is required. Your provider can contact CVS Customer Care to look up a specific drug to see if a prior authorization is required or for any other questions.
How do I manage balanced billing?
Balanced billing occurs when providers bill a patient for the difference between the amount they charge and the amount that the patient’s insurance approves. As an PASSE member and Arkansas Medicaid recipient, you are not responsible to pay any charges from your provider above the amount approved by Empower.
-
Providers
What is Empower Healthcare Solutions (Empower)?
Empower is one of four PASSE organizations in the state. We empower individuals to lead fuller, healthier lives at home and in their communities. PASSE (Provider-Led Arkansas Shared Savings Entity) is a Medicaid program to address the needs of individuals who have intensive behavioral health, intellectual disability, or developmental disability service needs.
Why is the PASSE program good for my patients?
The goal of the PASSE model is to improve the health of Arkansans who need intensive levels of specialized care due to behavioral health issues or developmental/intellectual disabilities. The PASSE model includes Care Coordination, which coordinates care for all community based services to improve total health outcomes for these members.
How do I update my roster?
To update your roster, please complete the Provider Roster Form located on the Providers page under “Provider Forms and Resources” and email to empower.network@empowerarkansas.com. If you have questions please contact Empower Provider Services at 855-429-1028.
How can I join Empower as a provider?
To become a participating provider with Empower, please complete the Empower Network Application located at the Providers Page under Forms and Resources and email to empower.network@empowerarkansas.com. If you have questions please contact Empower Provider Relations at 855-429-1028.
How do I join the Empower pharmacy network?
Empower is participating in the Caremark/CVS national network. If you are an AR pharmacy provider and in the Caremark/CVS national network then no action is needed. You can check the CVS national network here:
https://www.caremark.com/wps/myportal/PHARMACY_LOCATOR_FASTIf you are interested in joining the CVS network, you can start the process here:
https://www.caremark.com/wps/portal/FOR_HEALTH_PROS_HOME
Relevant links here include “Pharmacy Pre-Enrollment Questionnaire” and “Pharmacy Enrollment.”How do I verify Member Eligibility?
Empower member eligibility may change daily. Therefore, each participating provider is responsible for verifying eligibility with Empower before providing services to a member. Providers may verify eligibility using the following methods:
- Online – Visit our Business Operations Portal
- Telephone – Contact Provider Services at 1-855-429-1028.
What services require a PA?
Some services require a prior authorization from Empower for reimbursement to be issued. Please see Provider Forms and Resources on Empower’s website where there’s a link to a Quick Reference Guide for Key Contact Information and Prior Authorization for a list of services that require Prior Authorization.
Will I be required to report any quality measures for Empower?
Empower is committed to ensuring that continuous quality/performance improvement occurs. There is consistent and ongoing monitoring for applicability so Empower can achieve efficiency and effectiveness with improved outcomes for our members. HEDIS Measures will be used.
What are the rights of Empower Members?
Member Rights and Responsibilities are listed in the Member Handbook, available on the Empower website www.getempowerhealth.com.
What training will be provided to me as a PASSE provider and when?
Please check Empower’s Providers page and click Provider Training regularly for upcoming trainings and educational opportunities.
What are my rights and responsibilities as an Empower Provider?
Provider Rights and Responsibilities are in the Empower Provider Handbook, found on the Empower website www.getempowerhealth.com/for-providers/provider-materials/provider-handbook/.
How can I get a copy of the Empower Provider Manual?
The provider manual is available electronically on the Empower website, www.getempowerhealth.com/for-providers/provider-materials/provider-handbook/.
Who can answer questions about my contract as an Empower Provider?
You can contact the Empower network team at empower.network@empowerarkansas.com for help with questions about your Provider contract.
How do I know if an individual is a member of Empower?
All Empower members will have a member ID card. Members should always present their ID at the time of service, but an ID card, in and of itself, is not a guarantee of eligibility. Providers must verify a member’s eligibility on every date of service.

The ID card will contain the following information:
- Member’s name, Date of Birth, and Gender
- PASSE ID number
- Pharmacy ID number
- Empower contact information
- Claims filing address
How do Empower Members get a Primary Care Provider?
Members select their PCP when they sign up for Medicaid. Members who are also eligible for Medicare are able to keep their Medicare PCP. For any members who do not select a PCP, Empower will automatically assign a PCP based on:
- the member’s claims history (who they have seen in the past);
- a member’s geographical location;
- appropriate distribution by provider (so that members are not overly concentrated with the same PCP).
Members ages 18 and older will be assigned to a general or family practitioner, internal medicine, or other specialty provider approved by the state. Members under 18 years old will be assigned to a pediatrician or family practitioner. At any time, a member can call Empower Member Services and request that their PCP be changed, and Empower will honor that request if they are an In-Network provider.
What type of services are covered for Empower Members?
Empower members will be eligible for all services covered under the Medicaid state plan, as well as Section 1915(i) and CES waiver services, including therapy services and services through the Early Periodic Screening Diagnosis and Treatment (EPSDT) program for children. In short, members will have access to services covered under the Medicaid program today, as long as those services are deemed medically necessary and documented in the member’s Person Centered Service Plan (PCSP).
What services require an Extension of Benefits?
Some services have yearly benefit limits available before an Extension of Benefits request is required. Please see Prior Authorization Resources on Empower’s Providers page and clicking “Provider Forms and Resources” for benefit limits.
How do I submit a Prior Authorization (PA) or an Extension of Benefits?
Providers may submit Prior Authorizations in the following methods:
- Online – Visit our Business Operations Portal at https://bharportal.valence.care/
- Telephone – Contact Provider Services at 1-855-429-1028. Select option 2 for Utilization Management.
What is the process for submitting Pharmacy PAs, and what pharmacy services require a PA?
Empower is committed to providing appropriate, high quality, cost-effective drug therapy to all of our members. Empower works with providers and pharmacists to ensure that medications used to treat a variety of conditions and diseases are covered. The plan covers prescription drugs and certain over-the-counter (OTC) drugs when ordered by an Empower physician. The pharmacy program does not cover all medications. Some drugs have a generic equivalent or a brand-name drug from a different manufacturer that is covered. Some medications require prior authorization or have limitations on age, dosage, maximum quantities, or any combination of these.
Prior Authorization is necessary for some medications to establish medical necessity, and to ensure eligibility for coverage per State regulations, Federal regulations, or both. This may be due to specific Food and Drug Administration (FDA) indications, the potential for misuse or overuse, safety limitations, or cost- benefit justifications.
A PA is required for certain medications that are:
- Outside the recommended age, dose, or gender limits;
- Not listed on the Preferred Drug List (PDL);
- Listed on the PDL but still require Prior Authorization;
- Brand name drugs when a generic exists;
- A Duplication in therapy (i.e. another drug currently used within the same class);
- New to the market and not yet reviewed by the P&T Committee;
- Prescribed for off-label use or outside of certain diseases or specialties; or
- Self-injectable and infusion medications (including chemotherapy) with some exceptions.
Providers may request an exception to Empower’s PDL either verbally or in writing. For written requests, providers should complete a Prior Authorization Request Form that includes pertinent enrollee medical history and information. Prior Authorization Request Forms may be accessed on Empower’s Pharmacy Forms and Resources page.
If authorization cannot be approved or denied, and the drug is medically necessary, up to a 72-hour emergency supply of the drug can be supplied to the member.
How and when can I access information electronically about Empower Members?
Empower’s Business Operations Portal is available 24/7 and allows providers to instantly access many tools and resources. Providers and their office staff can register for our secure Business Operations Portal in just a few easy steps.
- Go to www.getempowerhealth.com
- Choose Business Operations from the Provider Home Page or Provider drop down
- Click ‘here’ to register
- Choose ‘Providers Click here’
- Register for Portal access
- Contracted Providers complete the web registration form.
- Out of Network Providers click ‘here’ under Provider Information to complete Portal Access Request
Once registered, the secure portal will allow you to:
- Request and track authorizations
- Submit claims and view payment history
- Verify member eligibility
- Review InterQual Criteria
How do I submit a claim and when can I submit a claim?
To make sure that Empower can process your claims in a timely manner, it is important that providers ensure Empower has accurate billing information on file. Providers must have a current, active Arkansas Medicaid Provider ID. Please confirm with Empower’s Network department (Empower.Network@empowerarkansas.com) that the following information is current in our files:
- Provider name (as noted on current W-9 form)
- National Provider Identifier (NPI)
- Tax Identification Number (TIN)
- Taxonomy code
- Physical location address (as noted on current W-9 form)
- Billing name and addres
For additional claims and payment information, please see Empower’s Provider Billing page.
I have additional questions about billing. Who can answer my questions and when can they answer them?
Empower’s Provider Services team will be available to help you via phone at 855-429-1028, Monday through Friday (except holidays), from 8:00 AM to 5:00 PM CT. You may also reach out to Empower’s Provider Relations Advocates for assistance by emailing EmpowerHealthcareSolutionsPR@empowerarkansas.com.